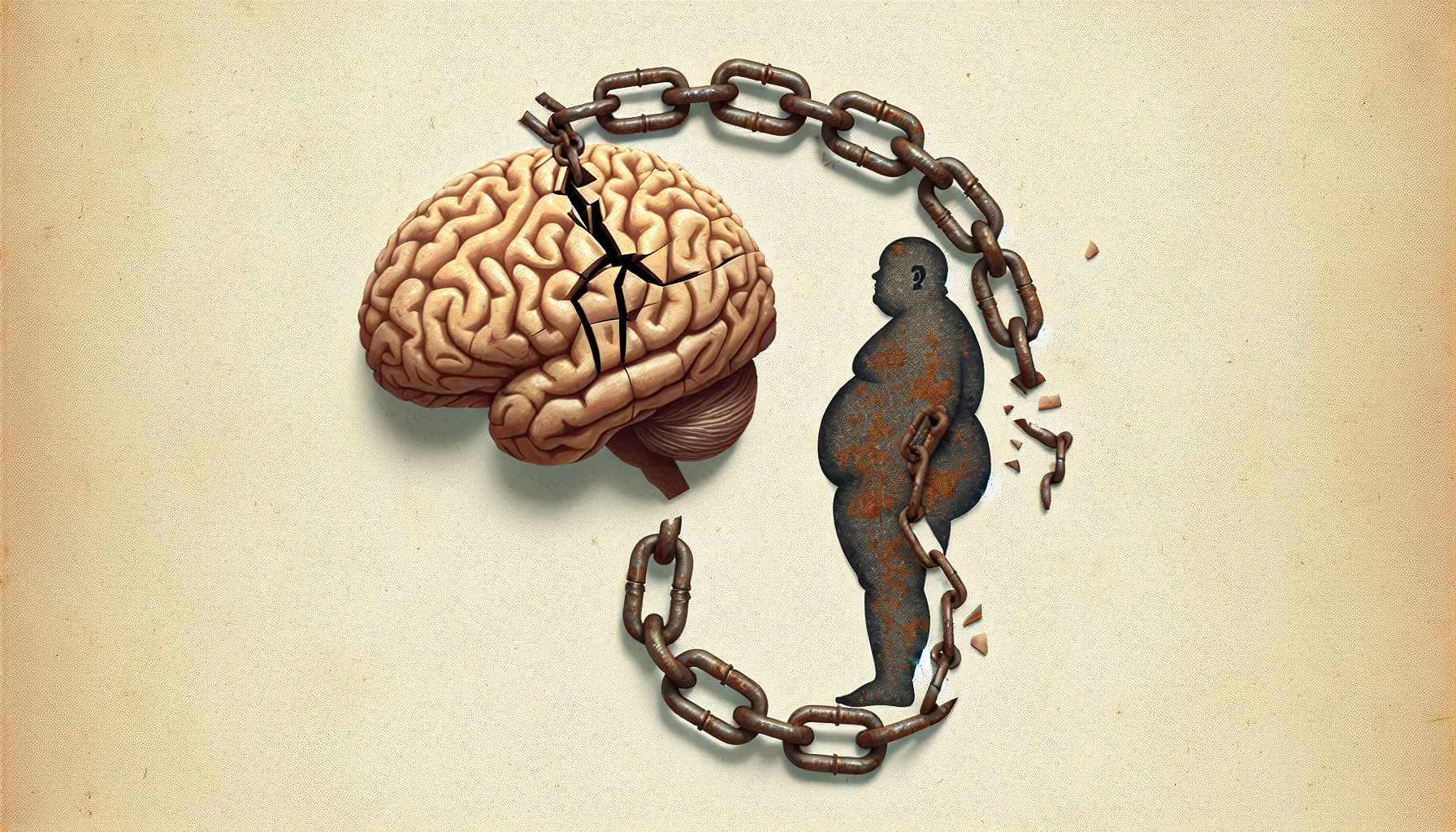
Are you aware of the potential link between obesity and mental health? Recent scientific studies have shed light on this intriguing connection, exploring how obesity can impact our mental well-being and mood disorders. A study published in the Journal of Clinical Endocrinology & Metabolism found that individuals with obesity were more likely to experience symptoms of depression and anxiety. Another study in JAMA Psychiatry revealed a bidirectional relationship between obesity and depression, where obesity increases the risk of depression, and depression in turn increases the risk of obesity. These findings offer a glimpse into the complex interplay between our physical and mental health, highlighting the importance of addressing both aspects for overall well-being.
Discover the Ultimate Weight Loss Secrets Here!
1. Connection between Obesity and Mental Health
The Link between Obesity and Depression
Obesity and depression have a complex relationship, with numerous studies suggesting that obesity can increase the risk of developing depression. A study published in the Journal of Psychiatric Research found that individuals with obesity were more likely to develop depression compared to those with normal weight. The reasons for this link are multifaceted, including both biological and psychological factors.
The Relationship between Obesity and Anxiety Disorders
Anxiety disorders, such as generalized anxiety disorder and panic disorder, are also associated with obesity. A review published in the Journal of Affective Disorders found that individuals with obesity were at an increased risk of developing anxiety disorders. The exact mechanisms behind this association are not yet fully understood, but hormonal imbalances and psychological factors are believed to play a role.
The Association between Obesity and Bipolar Disorder
Bipolar disorder is a mood disorder characterized by extreme mood swings, ranging from manic episodes to depressive episodes. Recent studies have highlighted a significant association between obesity and bipolar disorder. A study published in the International Journal of Bipolar Disorders found that individuals with bipolar disorder were more likely to be overweight or obese compared to the general population. This correlation emphasizes the need for further research to explore the possible underlying mechanisms.
2. Biological Mechanisms
Impact of Obesity on Brain Structure
Obesity has been shown to have direct effects on brain structure. Research published in the journal NeuroImage revealed that individuals with obesity had reduced gray matter volume in several brain regions, including the prefrontal cortex and hippocampus. These brain regions are involved in executive functions, memory, and emotional regulation, which may explain the higher incidence of mental health disorders in individuals with obesity.
Hormonal and Neurotransmitter Imbalances
Hormonal and neurotransmitter imbalances are common in individuals with obesity and can have profound effects on mental health. The hormone leptin, which is primarily produced by fat cells, plays a crucial role in regulating appetite and body weight. Dysregulation of leptin levels in individuals with obesity may impact mood and contribute to the development of mental health disorders. Additionally, imbalances in neurotransmitters such as serotonin and dopamine have been observed in individuals with obesity and are closely associated with mood regulation.
Inflammatory Processes and Oxidative Stress
Obesity is characterized by chronic low-grade inflammation and increased oxidative stress. These processes can have damaging effects on brain function and contribute to the development of mental health disorders. A study published in the journal Psychoneuroendocrinology found that markers of inflammation were significantly elevated in individuals with obesity and depression compared to those with obesity alone. The inflammatory response and oxidative stress may disrupt brain signaling pathways and contribute to the pathology of mental health disorders.
Click Here for Proven Fat-Burning Strategies!
3. Psychological Factors
Body Image Dissatisfaction
Body image dissatisfaction is a psychological factor that commonly affects individuals with obesity and can have a significant impact on mental health. Research published in the journal Eating and Weight Disorders showed that individuals who were dissatisfied with their bodies were more likely to experience symptoms of depression and anxiety. The societal emphasis on thinness and unrealistic beauty standards can contribute to body image dissatisfaction in individuals with obesity, leading to negative psychological outcomes.
Low Self-Esteem and Social Stigma
Low self-esteem is frequently observed in individuals with obesity, often as a result of societal stigma and discrimination. The negative attitudes and stereotypes associated with obesity can lead to feelings of shame, worthlessness, and social isolation. A study published in the Journal of Health Psychology found that low self-esteem mediated the relationship between obesity and symptoms of depression, suggesting that addressing self-esteem issues may be crucial for improving mental health outcomes in this population.
Emotional Eating and Food Addiction
Emotional eating, characterized by the consumption of food in response to negative emotions, is a common coping mechanism among individuals with obesity. It is often driven by psychological factors such as stress, sadness, or boredom. Emotional eating can contribute to weight gain and exacerbate mental health symptoms. Additionally, food addiction, which involves a loss of control over eating behaviors, has been associated with both obesity and mental health disorders. Understanding and addressing emotional eating patterns is essential in promoting better mental well-being in individuals with obesity.
4. Obesity as a Risk Factor for Mental Illness
Obesity as a Precursor to Mental Health Issues
While obesity and mental health disorders often coexist, research suggests that obesity can serve as a precursor to the development of mental health issues. A large-scale study published in JAMA Psychiatry followed over 2 million individuals and found a bidirectional relationship between obesity and depression, with individuals who were obese at baseline being at an increased risk of developing depression and vice versa. This highlights the importance of early intervention and preventive measures to address obesity as a potential risk factor for mental illness.
The Bidirectional Relationship between Obesity and Psychiatric Disorders
The relationship between obesity and psychiatric disorders is bidirectional, meaning that obesity can contribute to the development of mental health disorders, and vice versa. A longitudinal study published in the Archives of General Psychiatry found that obesity in adolescence predicted the development of mood and anxiety disorders in adulthood, while existing mood and anxiety disorders increased the risk of subsequent obesity. This bidirectional relationship emphasizes the need for comprehensive treatment strategies that address both obesity and mental health issues simultaneously.
Unlock Your Path to a Healthier You!
5. Obesity and Specific Mental Health Conditions
Depression and Obesity
Depression is one of the most common mental health disorders associated with obesity. A meta-analysis published in the International Journal of Obesity found that individuals with obesity had a significantly higher risk of developing depression compared to those with normal weight. The presence of depression can further complicate weight management efforts, making it essential to address both conditions in treatment plans.
Anxiety Disorders and Obesity
Anxiety disorders, such as generalized anxiety disorder and panic disorder, are frequently observed in individuals with obesity. A study published in Obesity Reviews reported that individuals with obesity had a 20% higher risk of developing anxiety disorders compared to those without obesity. Effective management of anxiety disorders in individuals with obesity can not only improve mental health outcomes but also support healthier weight management.
Bipolar Disorder and Obesity
Bipolar disorder, characterized by dramatic mood swings, is also associated with obesity. A study published in JAMA Psychiatry found a strong link between obesity and bipolar disorder, with individuals with bipolar disorder having a 1.3-fold higher risk of developing obesity compared to the general population. The complex interplay between obesity and bipolar disorder requires a comprehensive approach to treatment that addresses both physical and mental well-being.
6. Childhood Obesity and Mental Health
The Impact of Childhood Obesity on Mental Health
Childhood obesity has a significant impact on mental health and can lead to the development of various mental health conditions. A review published in Current Opinion in Psychiatry highlighted that children and adolescents with obesity are at an increased risk of experiencing depression, anxiety, and low self-esteem. Early intervention and prevention efforts are crucial in mitigating the long-term mental health consequences of childhood obesity.
Long-Term Effects of Childhood Obesity on Mental Well-being
The long-term effects of childhood obesity on mental well-being can extend into adulthood. A cohort study published in JAMA Pediatrics followed individuals from childhood to adulthood and found that obesity in adolescence was associated with an increased risk of developing mood and anxiety disorders in adulthood. Addressing childhood obesity not only promotes physical health but also has long-lasting benefits for mental well-being.
7. Treatment Approaches
Weight Loss Interventions and Improved Mental Health
Weight loss interventions have been shown to improve mental health outcomes in individuals with obesity. A randomized controlled trial published in JAMA Psychiatry demonstrated that a lifestyle intervention aimed at achieving weight loss resulted in significant improvements in symptoms of depression and anxiety. This highlights the importance of incorporating weight management strategies into the treatment of mental health disorders in individuals with obesity.
Integrated Treatment for Obesity and Mental Illness
Integrated treatment approaches that address both obesity and mental illness have shown promise in improving outcomes for individuals with comorbid conditions. A systematic review published in Obesity Reviews found that integrated interventions, combining dietary, physical activity, and psychological components, were effective in reducing both weight and symptoms of mental health disorders. Collaborative efforts between healthcare providers specializing in obesity and mental health are essential in providing holistic care for individuals with comorbid conditions.
8. Lifestyle Changes and Mental Well-being
Physical Activity and Mental Health Benefits
Engaging in regular physical activity has numerous mental health benefits for individuals with obesity. Research published in the American Journal of Preventive Medicine showed that exercise interventions had a positive impact on symptoms of depression and anxiety in this population. Physical activity promotes the release of endorphins, improves self-esteem, and provides a healthy coping mechanism for stress and negative emotions.
Healthy Diet and its Impact on Mood Disorders
A healthy diet has been associated with better mental health outcomes in individuals with obesity. A study published in the Journal of Clinical Psychopharmacology demonstrated that a Mediterranean-style diet, rich in fruits, vegetables, whole grains, and lean proteins, was effective in reducing depressive symptoms. Nutritional interventions that focus on improving dietary quality can have a profound impact on both physical and mental well-being.

9. Strategies for Healthcare Providers
Screening and Assessment of Mental Health in Obese Individuals
Healthcare providers play a vital role in identifying and addressing mental health issues in individuals with obesity. Regular screening and assessment of mental health should be included as part of routine care for individuals with obesity. Screening tools, such as the Patient Health Questionnaire (PHQ-9) for depression and the Generalized Anxiety Disorder 7-item scale (GAD-7) for anxiety, can help identify symptoms and guide appropriate interventions.
Multidisciplinary Collaboration between Mental Health and Obesity Specialists
Multidisciplinary collaboration between mental health and obesity specialists is crucial in providing comprehensive care for individuals with comorbid conditions. Effective communication and coordination between healthcare providers from various disciplines, including psychiatry, psychology, endocrinology, and nutrition, can ensure that treatment plans address both the physical and mental health needs of individuals with obesity.
10. Conclusion
The connection between obesity and mental health is complex and multifaceted. Both biological mechanisms and psychological factors contribute to the increased risk of mental health disorders among individuals with obesity. Recognizing the bidirectional relationship between obesity and psychiatric conditions is essential in providing optimal care. Integrated treatment approaches that combine weight management strategies and mental health interventions hold promise in improving outcomes for individuals with comorbid conditions. By addressing the interplay between obesity and mental health, healthcare providers can make a significant impact on the well-being of individuals dealing with these challenges.