We all know that obesity can have a negative impact on our overall health, but have you ever wondered how it affects our immune response? Recent scientific studies have shed light on this very question, revealing some intriguing findings. One study conducted by researchers at the University of California, San Francisco, found that obesity can impair the function of immune cells, making them less effective at fighting off infections. Another study from the University of Michigan discovered that obesity can lead to chronic inflammation in the body, which can weaken the immune system and increase the risk of various diseases. These studies provide valuable insights into the complex relationship between obesity and our body’s defense mechanisms, highlighting the importance of maintaining a healthy weight for optimal immune function.
Discover the Ultimate Weight Loss Secrets Here!
Background on Obesity and Immune System
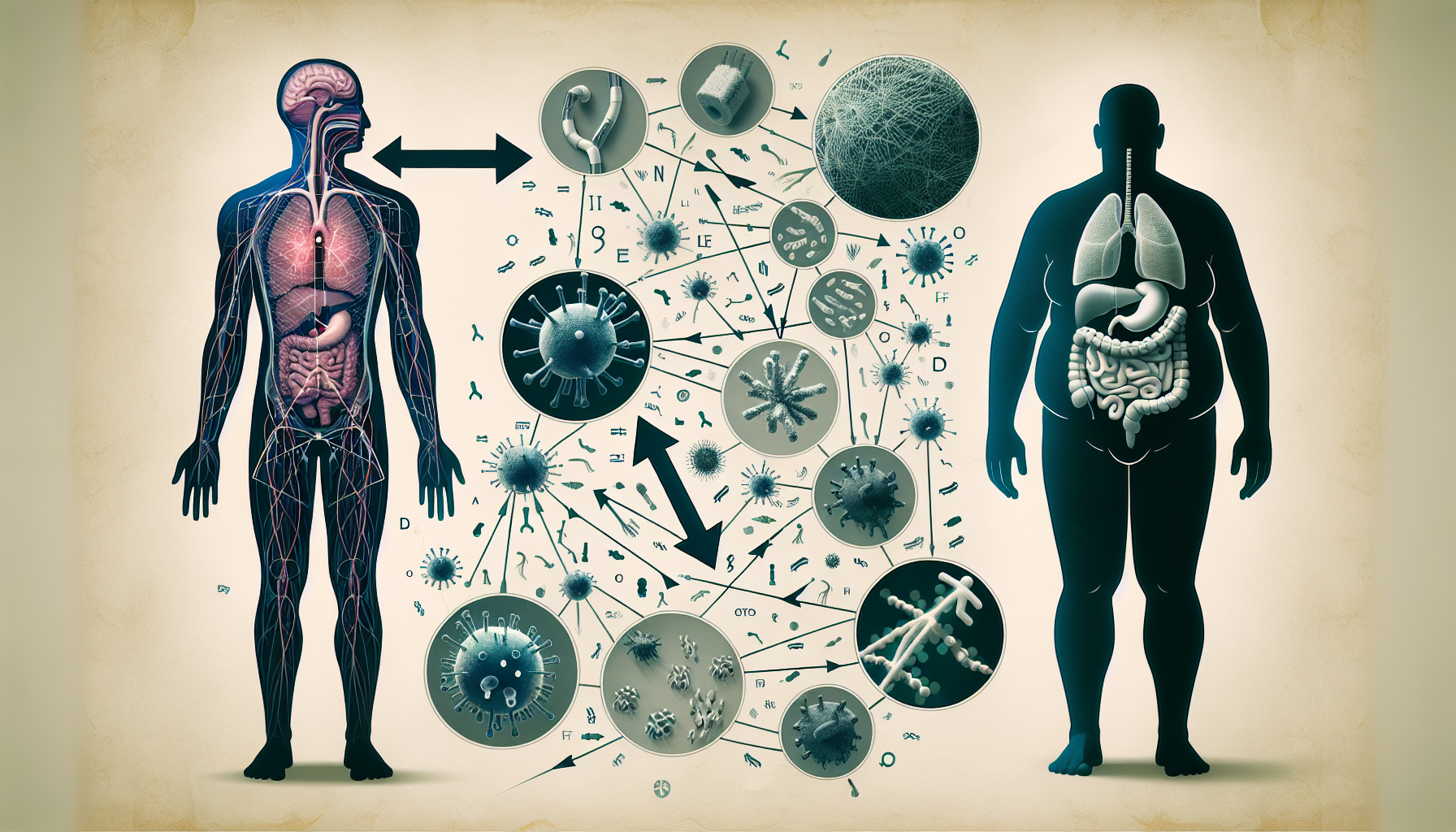
Obesity is a condition characterized by excessive body fat accumulation, which can have detrimental effects on various aspects of health, including the immune system. The immune system is a complex network of organs, cells, and molecules that work together to defend the body against pathogens and maintain its overall health. It plays a crucial role in identifying and eliminating foreign invaders, as well as in regulating inflammation and promoting tissue repair.
Definition of obesity
Obesity is typically defined based on Body Mass Index (BMI), which is calculated using an individual’s weight and height. A BMI of 30 or higher is considered indicative of obesity. However, it is important to note that BMI is a general measure and may not accurately reflect an individual’s body fat percentage or overall health.
Overview of the immune system
The immune system can be divided into two main branches: the innate immune system and the adaptive immune system. The innate immune system provides an immediate, nonspecific response to pathogens through the activation of various cells, such as macrophages and neutrophils, and the release of inflammatory molecules. On the other hand, the adaptive immune system provides a more specific response to pathogens by producing antibodies and activating lymphocytes, such as T cells and B cells.
Impact of Obesity on Immune Cells
Altered number and function of immune cells
Obesity has been shown to alter both the number and function of immune cells in the body. Studies have indicated that obese individuals often have increased levels of pro-inflammatory immune cells, such as macrophages and T cells, in their adipose tissue. These immune cells can release excessive amounts of inflammatory molecules, leading to a chronic low-level inflammation in the body, which we will discuss further in subsequent sections.
Additionally, obesity can also lead to a decrease in the number of regulatory T cells, which play a crucial role in maintaining immune balance and preventing excessive immune responses. This imbalance in immune cell populations can disrupt immune regulation and contribute to the development of various diseases.
Inflammatory response
One of the key consequences of obesity on the immune system is the promotion of chronic low-grade inflammation. Adipose tissue, particularly visceral adipose tissue, is an active endocrine organ that secretes various bioactive molecules, collectively known as adipokines. In obese individuals, the adipose tissue expands and dysregulates the production of adipokines, including pro-inflammatory molecules such as tumor necrosis factor-alpha (TNF-alpha) and interleukin-6 (IL-6).
The elevated levels of these pro-inflammatory molecules can disrupt the balance between pro-inflammatory and anti-inflammatory signals in the body, leading to systemic inflammation. Chronic low-grade inflammation is associated with a range of health conditions, including insulin resistance, cardiovascular disease, and autoimmune disorders.
Click Here for Proven Fat-Burning Strategies!
Obesity-Related Inflammation
Chronic low-grade inflammation
As previously mentioned, obesity-induced inflammation is characterized by a chronic low-level activation of the immune system. This ongoing inflammatory response can have far-reaching effects on various organ systems and contribute to the development of metabolic disorders, such as type 2 diabetes and non-alcoholic fatty liver disease.
Recent studies have shown that obesity-related chronic inflammation is not limited to adipose tissue but can also affect other tissues and organs, including the liver, pancreas, and skeletal muscle. This systemic inflammation can impair organ function, disrupt metabolic homeostasis, and contribute to the development of obesity-related complications.
Role of adipose tissue in inflammation
Adipose tissue is not just an energy storage depot; it also plays a critical role in modulating systemic inflammation. Adipocytes, or fat cells, secrete adipokines, which can either promote or dampen inflammation. In obesity, the adipose tissue becomes dysfunctional and produces increased levels of pro-inflammatory adipokines, such as TNF-alpha, IL-6, and leptin. These adipokines can directly contribute to insulin resistance, cellular stress, and immune cell activation, further exacerbating the inflammatory response.
Moreover, adipose tissue in obesity undergoes significant structural changes, including an increase in the size and number of adipocytes, infiltration of immune cells, and remodeling of the extracellular matrix. These changes enhance the production and release of inflammatory molecules, perpetuating the cycle of chronic inflammation.
Link between obesity-related inflammation and immune response
The immune system and inflammation are intricately connected, and obesity-induced inflammation can have profound effects on immune cell function. Chronic low-grade inflammation can disrupt the balance between pro-inflammatory and anti-inflammatory signals, leading to impaired immune responses and dysregulated immune cell function.
Several studies have shown that obesity alters the phenotype and function of immune cells, such as neutrophils, macrophages, and T cells. Obesity-related inflammation can promote the polarization of macrophages towards a pro-inflammatory state, impair the phagocytic capacity of immune cells, and modulate T cell responses. These alterations in immune cell behavior contribute to the development of obesity-related metabolic disorders and increase the risk of infections and autoimmune diseases.
Effects on Innate Immunity
Impaired innate immune response
The innate immune system acts as the first line of defense against pathogens, and obesity can impair its overall function. Studies have shown that obese individuals exhibit impaired innate immune responses, making them more susceptible to infections.
Obesity can affect the function of key innate immune cells, such as macrophages and neutrophils, compromising their ability to recognize and eliminate pathogens effectively. Furthermore, the excessive release of pro-inflammatory adipokines in obesity can further dysregulate the immune response, contributing to impaired innate immune defenses.
Defective phagocytosis
Phagocytosis is an essential process by which immune cells engulf and eliminate pathogens, cellular debris, and other foreign substances. Obesity has been associated with defective phagocytosis, primarily mediated by impaired macrophage and neutrophil function.
Studies have shown that obese individuals have reduced phagocytic capacity in response to bacterial infections and impaired clearance of apoptotic cells. This defect in phagocytosis can delay the resolution of inflammation and contribute to the development of chronic infections and inflammatory disorders.
Increased susceptibility to infections
The impaired innate immune response and defective phagocytosis observed in obesity can increase an individual’s susceptibility to infections. Obese individuals may experience more frequent and severe infections, including respiratory tract infections, skin infections, and urinary tract infections.
Moreover, obesity-related inflammation can impair the production and effectiveness of antimicrobial peptides, further compromising the body’s ability to defend against pathogens. These immune deficiencies can have significant implications for the health and well-being of obese individuals, highlighting the importance of addressing obesity as a risk factor for infectious diseases.
Unlock Your Path to a Healthier You!
Effects on Adaptive Immunity
Altered lymphocyte response
Adaptive immunity, mediated by lymphocytes, plays a crucial role in the recognition and elimination of specific pathogens. Obesity has been shown to alter lymphocyte responses, leading to dysregulated immune function.
Studies have demonstrated that obese individuals often exhibit altered lymphocyte distribution, with a decrease in the number of naive T cells and an increase in memory T cells. This shift in the balance between naive and memory T cells can affect the ability to mount appropriate immune responses, particularly in the context of novel infections.
Reduced vaccine efficacy
Vaccines are a vital tool in preventing infectious diseases, relying on the adaptive immune system to generate protective immune responses. However, obesity can negatively impact vaccine efficacy and immune memory.
Research has indicated that obese individuals may have reduced vaccine responses, resulting in lower antibody production and a decreased ability to generate long-term immune memory. This reduced vaccine efficacy can leave obese individuals more vulnerable to vaccine-preventable diseases and reduce the overall effectiveness of vaccination campaigns in populations with high obesity rates.
Increased risk of autoimmune diseases
Autoimmune diseases occur when the immune system mistakenly attacks its own tissues. Obesity has been associated with an increased risk of developing autoimmune diseases, such as rheumatoid arthritis, systemic lupus erythematosus, and multiple sclerosis.
The exact mechanisms underlying the link between obesity and autoimmune diseases are not yet fully understood. However, it is believed that the chronic low-grade inflammation associated with obesity can promote immune dysregulation and break down immune tolerance, leading to the development of self-reactive immune responses.
Obesity and Immunosenescence
Premature aging of the immune system
Immunosenescence refers to the gradual deterioration of the immune system that occurs with age. Obesity has been shown to accelerate the aging process of the immune system, leading to premature immunosenescence.
Studies have demonstrated that obese individuals, even at a relatively young age, exhibit immune changes typically associated with older individuals. These changes include decreased production of immune cells, reduced diversity in the T cell repertoire, and impaired immune responses to infections and vaccinations.
Impaired immune response in older obese individuals
In older obese individuals, the combination of age-related immune decline and obesity-related immune dysregulation can have a severe impact on immune function. Aging already leads to a decreased ability to respond to infections and increased susceptibility to diseases. When coupled with obesity, this impaired immune response becomes even more pronounced.
Older obese individuals may experience reduced vaccine responses, delayed wound healing, and an increased risk of complications from infections. The synergistic effects of aging and obesity on the immune system highlight the importance of maintaining a healthy weight throughout the lifespan to preserve immune function and reduce the risk of infectious and age-related diseases.
Obesity and Immune-Related Disorders
Obesity-associated asthma
Obesity has emerged as a significant risk factor for the development and severity of asthma. Recent studies have shown a strong association between obesity and asthma, with obese individuals being more likely to develop asthma and experience worse symptoms.
The mechanisms underlying the link between obesity and asthma are multifactorial and involve both mechanical and immune-related factors. Obesity-induced inflammation can contribute to airway hyperresponsiveness, mucus production, and airway remodeling, all of which can worsen asthma symptoms. Additionally, adipokines and other inflammatory molecules may directly influence the inflammatory cascade in the airways, further exacerbating asthma pathophysiology.
Obesity-related autoimmune diseases
Obesity has been associated with an increased risk of developing various autoimmune diseases, such as rheumatoid arthritis, psoriasis, and inflammatory bowel disease.
Recent research has shown that obesity-related inflammation can contribute to the development and progression of autoimmune diseases by promoting immune dysregulation and the breakdown of self-tolerance. Adipose tissue-derived inflammation may trigger or exacerbate autoimmune responses in susceptible individuals, leading to the development of these chronic inflammatory conditions.
Obesity and cancer
Obesity and cancer are both major public health concerns, and recent studies have revealed a strong link between the two. Obesity has been identified as a significant risk factor for various types of cancer, including breast, colorectal, and endometrial cancer.
Mechanisms underlying the association between obesity and cancer involve complex interactions between adipose tissue, inflammatory processes, and metabolic dysregulation. Adipose tissue can secrete bioactive molecules that promote tumor growth, angiogenesis, and metastasis. Additionally, obesity-related inflammation can directly influence the tumor microenvironment and immune surveillance, compromising the body’s ability to recognize and eliminate cancer cells.
Gut Microbiota and Immune Response
Imbalance in gut microbiota composition
The gut microbiota plays a critical role in immune system regulation, and its composition can be significantly altered in obesity. Recent studies have shown that obesity is associated with an imbalance in gut microbiota composition, characterized by a reduction in microbial diversity and altered abundance of specific bacterial species.
This dysbiosis in the gut microbiota can influence immune function, as certain bacteria promote anti-inflammatory responses while others drive pro-inflammatory pathways. The altered gut microbiota composition in obesity can contribute to systemic low-grade inflammation, impair immune cell function, and increase the risk of metabolic disorders.
Effect on immune system regulation
The gut microbiota interacts with the immune system through various mechanisms, including the production of microbial metabolites, regulation of intestinal barrier function, and modulation of immune cell development and activity.
Obesity-associated changes in the gut microbiota composition can disrupt immune system regulation. Dysbiosis can lead to increased production of pro-inflammatory metabolites, disruption of the intestinal barrier, and an imbalance in immune cell populations. These alterations can have a profound impact on immune responses, promoting inflammation and contributing to the development of obesity-related complications.
Impact of Weight Loss on Immune Function
Improvement in immune cell profile
Weight loss has been shown to positively impact immune cell profile and function in obese individuals. Studies have demonstrated that weight loss, achieved through caloric restriction or bariatric surgery, can lead to a reduction in pro-inflammatory immune cells and an increase in regulatory immune cell populations.
Additionally, weight loss has been associated with improved immune cell function, including enhanced phagocytic capacity and immune response to infections. These improvements in immune cell profile and function may contribute to the reduction of chronic low-grade inflammation observed following weight loss.
Reduction in inflammation
Weight loss has a significant impact on reducing systemic low-grade inflammation in obese individuals. Studies have consistently shown that weight loss leads to a decrease in circulating inflammatory markers, such as C-reactive protein (CRP) and IL-6.
The reduction in chronic inflammation is believed to be mediated by the decrease in adipose tissue mass, particularly visceral adipose tissue. As adipose tissue decreases, the production of pro-inflammatory adipokines decreases, restoring the balance between pro-inflammatory and anti-inflammatory signals in the body. This reduction in inflammation is crucial for improving overall health and reducing the risk of obesity-related complications.
Enhanced immune response
Weight loss has also been associated with an enhanced immune response in obese individuals. Studies have shown that weight loss improves vaccine responses, with increased antibody production and a more robust immune memory.
Furthermore, weight loss can restore the phagocytic capacity of immune cells, promoting effective pathogen elimination and reducing the risk of infections. The improvements in immune function following weight loss are essential for maintaining a healthy immune system and reducing the susceptibility to diseases.
Conclusion
Obesity has a profound impact on the immune system, leading to alterations in immune cell function, chronic inflammation, and an increased risk of immune-related disorders. The chronic low-grade inflammation associated with obesity can disrupt immune regulation and impair immune response to infections, vaccines, and tumors. Additionally, obesity-related changes in gut microbiota composition further contribute to immune dysregulation and systemic inflammation.
Understanding the complex interactions between obesity and the immune system is critical for developing strategies to mitigate the negative effects of obesity on immune function. Promoting weight loss, through lifestyle modifications or medical interventions, can lead to improvements in immune cell profile, reduction in inflammation, and enhanced immune response. By addressing obesity and its impact on the immune system, we can improve overall health outcomes and reduce the burden of obesity-related complications.

