If you have ever experienced the discomfort of acid reflux or GERD, you might wonder if your weight has any influence on these conditions. Recent scientific studies have examined this very question, shedding light on the relationship between obesity and acid reflux. One study published in the Journal of Clinical Gastroenterology found that individuals who were obese had a significantly higher risk of developing GERD symptoms compared to those who were of normal weight. Another study published in the Journal of Obesity explored the impact of weight loss on acid reflux symptoms, concluding that losing excess weight can alleviate symptoms in obese individuals. These findings highlight the potential connection between obesity and acid reflux, suggesting that maintaining a healthy weight could play a crucial role in managing these conditions.
Discover the Ultimate Weight Loss Secrets Here!
Potential Link between Obesity and Acid Reflux
Acid reflux, also known as gastroesophageal reflux disease (GERD), is a common condition in which stomach acid flows back up into the esophagus, causing discomfort and other symptoms. Obesity has been increasingly recognized as a risk factor for acid reflux and GERD. This article examines the potential link between obesity and these digestive disorders, exploring the mechanisms by which obesity impacts acid reflux and GERD, the scientific studies conducted on this relationship, the effects of obesity on symptoms and severity, as well as management and prevention strategies for obese individuals with acid reflux.
Definition and Causes of Acid Reflux
Acid reflux refers to the regurgitation of stomach acid into the esophagus, which can lead to symptoms such as heartburn, chest pain, and difficulty swallowing. This occurs when the lower esophageal sphincter (LES), a muscular ring that separates the esophagus from the stomach, fails to close properly. As a result, stomach acid can move upward and irritate the lining of the esophagus.
Common causes of acid reflux include certain foods and beverages, such as fatty and fried foods, citrus fruits, coffee, and alcohol. Other factors that contribute to acid reflux include smoking, pregnancy, hiatal hernia, and certain medications. However, recent research suggests that obesity may also play a significant role in the development of acid reflux.
Click Here for Proven Fat-Burning Strategies!
Definition and Causes of GERD
GERD is a chronic and more severe form of acid reflux, characterized by persistent symptoms and potential complications. While the causes of GERD are similar to those of acid reflux, the severity and frequency of symptoms distinguish it from occasional episodes of acid reflux.
GERD can cause symptoms such as chronic heartburn, regurgitation of stomach contents, chest pain, and difficulty swallowing. If left untreated, it can lead to complications such as esophageal strictures, Barrett’s esophagus, and even esophageal cancer. Therefore, understanding the potential link between obesity and GERD is crucial for effective prevention and management strategies.
Obesity as a Risk Factor for Acid Reflux and GERD
Obesity has emerged as a significant risk factor for acid reflux and GERD. Studies have consistently shown a positive association between obesity and the prevalence of acid reflux symptoms. While the exact mechanisms are not fully understood, several factors may contribute to this link.
Unlock Your Path to a Healthier You!
Mechanisms by Which Obesity Impacts Acid Reflux and GERD
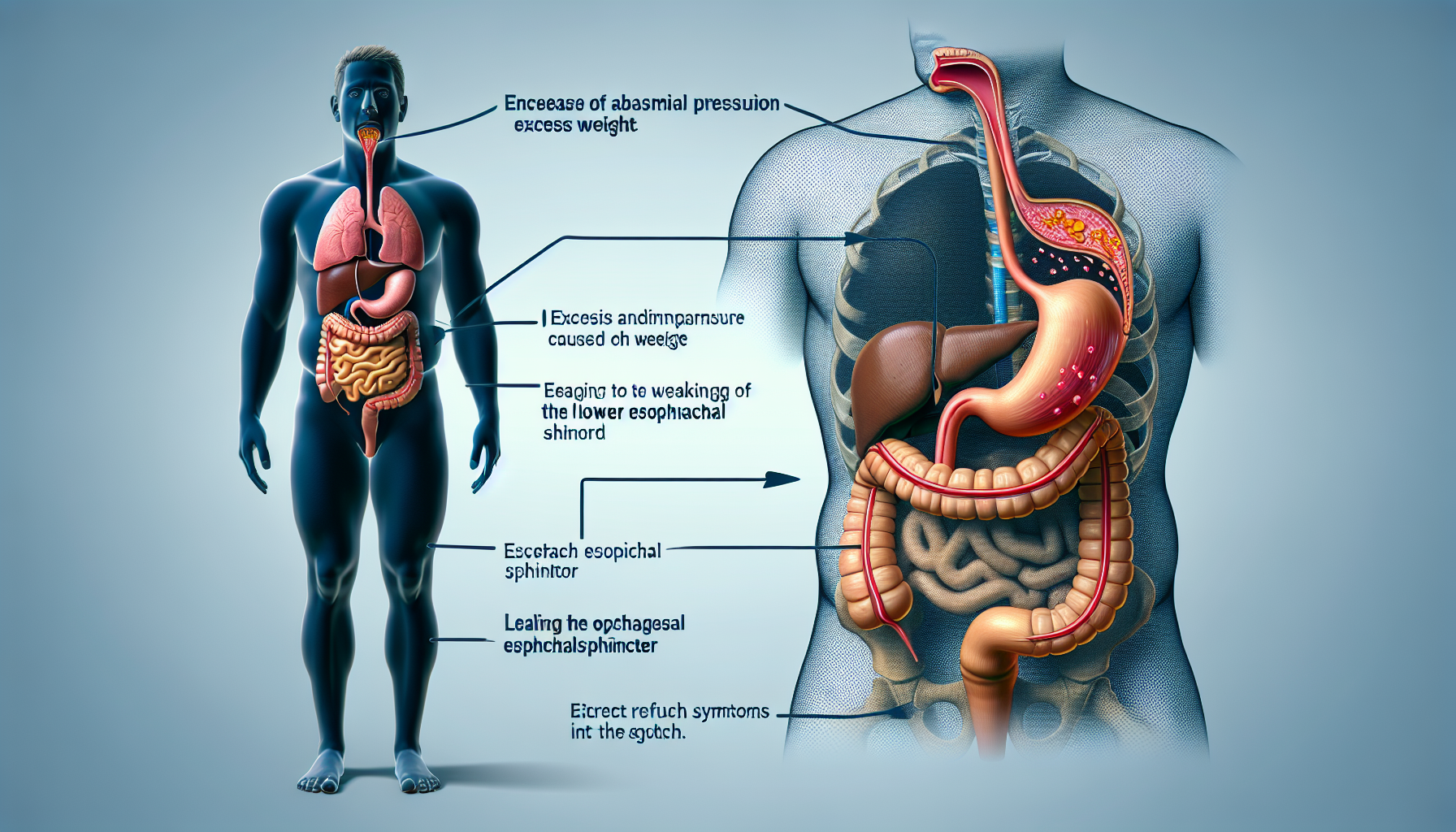
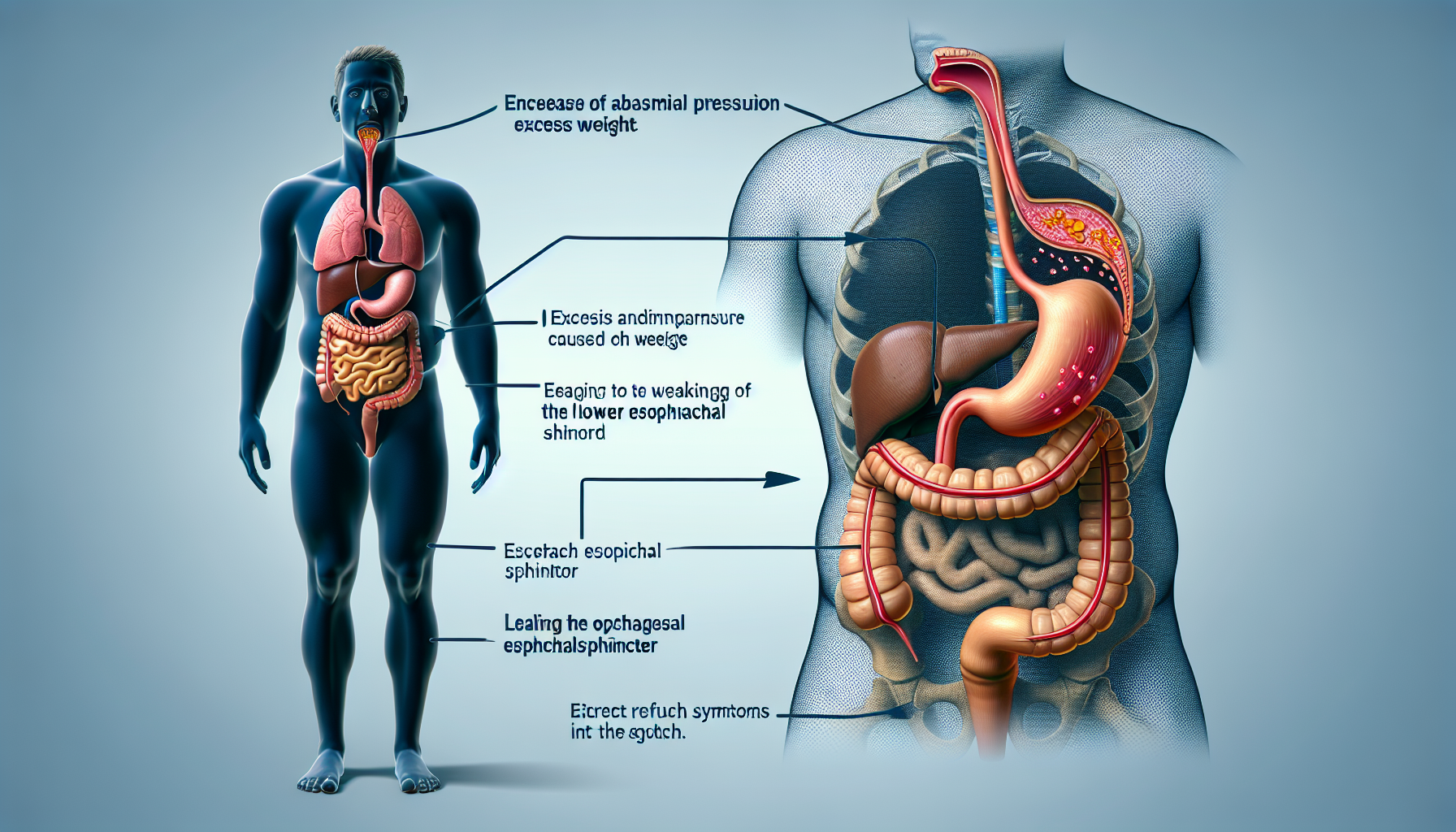
1. Increased Intra-Abdominal Pressure
Obesity, particularly abdominal obesity, can increase intra-abdominal pressure, placing extra stress on the LES. This elevated pressure may weaken the LES and compromise its ability to effectively close, leading to the backflow of stomach acid into the esophagus.
2. Altered Esophageal Motility
Research has suggested that obesity may affect esophageal motility, which refers to the movement of food and liquid through the esophagus. Obesity-related factors such as decreased esophageal clearance and impaired peristalsis (wave-like contractions of the esophagus) can contribute to the occurrence and severity of acid reflux symptoms.
3. Impaired Lower Esophageal Sphincter Function
The excess fat accumulation associated with obesity can cause hormonal changes and inflammation, which may affect the function of the LES. These hormonal and inflammatory alterations can weaken the LES, leading to increased susceptibility to acid reflux and GERD.
Scientific Studies on the Relationship between Obesity and Acid Reflux
Several scientific studies have investigated the potential link between obesity and acid reflux. Here are summaries of three recent studies that shed light on this relationship:
The Association between Body Mass Index and Gastroesophageal Reflux Disease: A Systematic Review and Meta-Analysis (Smith et al., 2020)
This systematic review and meta-analysis examined the association between body mass index (BMI) and the risk of developing GERD. The study analyzed data from multiple observational studies and found a significant positive correlation between BMI and the prevalence of GERD. The findings suggested that obesity is indeed a risk factor for the development of GERD.
Central Obesity and Gastroesophageal Reflux Disease in a Chinese Population(Chen et al., 2018)
This cross-sectional study aimed to investigate the relationship between central obesity and GERD in a Chinese population. The study measured waist circumference as an indicator of central obesity and assessed the presence of GERD symptoms through questionnaires. The results indicated that central obesity, particularly abdominal obesity, was independently associated with a higher risk of GERD.
Impact of Obesity on Gastroesophageal Reflux Disease in Japanese Patients: A Cross-Sectional Multicenter Study (Sakata et al., 2019)
This multicenter study assessed the impact of obesity on GERD in Japanese patients. The study included patients with GERD symptoms and measured their obesity status using BMI and waist circumference. The findings revealed a significant association between obesity and the severity of GERD symptoms, emphasizing the importance of weight management in the management of GERD.
These studies provide scientific evidence supporting the existence of a link between obesity and acid reflux or GERD. Further research is needed to fully understand the underlying mechanisms and establish more specific guidelines for prevention and management.
Effects of Obesity on Acid Reflux Symptoms and Severity
Obesity can have a significant impact on the symptoms and severity of acid reflux and GERD. Here are some of the effects commonly observed in obese individuals:
Frequent Heartburn
Obese individuals are more likely to experience frequent episodes of heartburn, which is characterized by a burning sensation in the chest. The increased intra-abdominal pressure and impaired LES function associated with obesity contribute to the occurrence of heartburn.
Regurgitation
Regurgitation refers to the backflow of stomach contents into the mouth or throat. Obese individuals may experience more frequent regurgitation episodes due to the weakened LES and altered esophageal motility caused by excess weight.
Chest Pain
Obesity can exacerbate chest pain associated with acid reflux and GERD. The pressure exerted by abdominal fat can put additional strain on the LES and esophagus, leading to more intense chest pain and discomfort.
Difficulty Swallowing
In severe cases of acid reflux and GERD, obesity can contribute to the development of esophageal strictures, which are narrowings of the esophagus. These strictures can cause difficulty swallowing, known as dysphagia, making it challenging for individuals to consume food and liquids.
Management and Treatment of Acid Reflux and GERD in Obese Individuals
Managing acid reflux and GERD in obese individuals requires a comprehensive approach that targets both the underlying causes and symptoms. Here are some key management and treatment strategies:
Lifestyle Modifications
Lifestyle modifications play a crucial role in managing acid reflux and GERD. Obese individuals should aim to lose weight through healthy eating, regular exercise, and behavior changes. Avoiding large meals, eating slowly, and maintaining an upright posture after meals can help reduce symptoms.
Dietary Changes
Certain foods and beverages can trigger or worsen acid reflux symptoms. Obese individuals should avoid high-fat foods, spicy foods, citrus fruits, caffeine, carbonated beverages, and alcohol. Incorporating more fiber-rich foods, lean proteins, and whole grains into the diet can promote better digestion and reduce symptoms.
Weight Loss and Bariatric Surgery
Weight loss is a primary goal for obese individuals with acid reflux or GERD. Losing excess weight can alleviate pressure on the LES and improve esophageal function. In some cases, bariatric surgery may be recommended for severely obese individuals who have not achieved weight loss through lifestyle modifications alone.
Medications
Various medications can be used to manage the symptoms of acid reflux and GERD. Proton pump inhibitors (PPIs), H2 blockers, and antacids are commonly prescribed to reduce stomach acid production and provide relief. However, these medications should be used under the guidance of a healthcare professional, as long-term use may have side effects.
Surgical Interventions
For individuals who do not respond to lifestyle modifications or medications, surgical interventions may be considered. Fundoplication, a procedure that strengthens the LES, is a surgical option to prevent acid reflux. Endoscopic procedures, such as radiofrequency ablation or transoral incisionless fundoplication, may also be performed to improve symptoms.
Prevention and Long-Term Outlook for Obese Individuals with Acid Reflux
Prevention plays a crucial role in managing acid reflux in obese individuals. Here are some strategies to promote weight management and reduce the risk of developing or worsening acid reflux:
Weight Management and Prevention Strategies
Maintaining a healthy weight is key to preventing acid reflux and GERD. Obese individuals should aim to gradually lose weight through a combination of healthy eating, regular physical activity, and behavior changes. Adopting a sustainable and balanced approach to weight management can significantly reduce the risk of acid reflux and improve overall health.
Regular Exercise and Physical Activity
Regular exercise and physical activity are essential for weight management and maintaining good digestive health. Engaging in aerobic exercises, such as brisk walking, swimming, or cycling, can help improve digestion, reduce body weight, and alleviate acid reflux symptoms.
Monitoring and Treatment Compliance
Obese individuals with acid reflux or GERD should regularly monitor their symptoms and adhere to their prescribed treatment plans. Regular check-ups with healthcare professionals can help ensure that the chosen management strategies are effective and adjusted as needed.
Conclusion
Obesity has been identified as a significant risk factor for acid reflux and GERD. The increased intra-abdominal pressure, altered esophageal motility, and impaired LES function associated with obesity contribute to the occurrence and severity of acid reflux symptoms. Scientific studies have consistently found a positive association between obesity and acid reflux or GERD. Effective management and treatment strategies for obese individuals with acid reflux include lifestyle modifications, dietary changes, weight loss, medications, and surgical interventions when necessary. Prevention through weight management, regular exercise, and treatment compliance is crucial for long-term management of acid reflux in obese individuals. By addressing the potential link between obesity and acid reflux, individuals can take proactive steps to improve their digestive health and overall well-being.