As you go through life, have you ever wondered how age impacts your blood pressure? Recent scientific studies have sought to answer this very question, shedding light on the relationship between age and blood pressure. One study conducted by researchers at the Northwestern University Feinberg School of Medicine found that blood pressure tends to rise gradually as a person gets older, with the risk of hypertension increasing significantly with age. Another study published in the Journal of the American Heart Association discovered that even small increases in blood pressure during midlife can significantly raise the risk of cardiovascular disease later in life. These studies provide valuable insights into the complex interplay between age and blood pressure, highlighting the importance of monitoring and managing this vital aspect of your health as you age.

Discover the Ultimate Weight Loss Secrets Here!
Understanding Blood Pressure
What is blood pressure?
Blood pressure refers to the force exerted by the blood against the walls of the blood vessels as it circulates through the body. It is measured in millimeters of mercury (mmHg) and is expressed as two numbers: systolic pressure over diastolic pressure. The systolic pressure represents the force when the heart contracts, while the diastolic pressure represents the force when the heart is at rest between beats.
Why is blood pressure important?
Blood pressure is a vital indicator of cardiovascular health. It helps determine the workload on the heart and the efficiency of blood flow throughout the body. Maintaining a healthy blood pressure range is crucial for preventing various cardiovascular conditions, including heart disease, stroke, and kidney problems.
Blood pressure measurements
Blood pressure is typically measured using a device called a sphygmomanometer. The measurements are recorded as two numbers, such as 120/80 mmHg. The first number is the systolic pressure, and the second number is the diastolic pressure. These readings provide healthcare professionals with valuable information about a person’s cardiovascular health and help diagnose conditions like hypertension.
Normal Blood Pressure Range
Systolic and diastolic pressure
The systolic pressure is the higher number in a blood pressure reading and represents the pressure in the arteries when the heart contracts. The diastolic pressure, on the other hand, is the lower number and signifies the pressure in the arteries when the heart is at rest. The normal blood pressure range for adults is typically around 120/80 mmHg. However, individual variations and specific medical conditions can influence what is considered normal for some individuals.
Factors affecting blood pressure
Several factors can affect blood pressure levels. These include age, gender, genetics, lifestyle choices, underlying medical conditions, stress levels, and certain medications. It is important to consider these factors when interpreting blood pressure readings and evaluating an individual’s cardiovascular health.
Click Here for Proven Fat-Burning Strategies!
Effect of Age on Blood Pressure
Blood pressure changes with age
As people age, their blood pressure tends to increase gradually. This increase is due to various physiological changes that occur in the cardiovascular system over time. It is essential to understand these age-related changes to identify potential risk factors and manage blood pressure effectively.
Development of hypertension
Hypertension, or high blood pressure, is more prevalent among older adults. It often develops gradually over the course of several years as a result of cumulative damage to blood vessels and the heart. Age-related hypertension is a significant concern as it increases the risk of cardiovascular diseases and other related complications.
Age-Related Hypertension
Definition and symptoms
Age-related hypertension refers to high blood pressure that occurs as a person gets older. It is typically characterized by systolic blood pressure consistently reaching 140 mmHg or higher and diastolic blood pressure consistently reaching 90 mmHg or higher. Symptoms of hypertension may not always be apparent, which is why regular blood pressure monitoring is crucial for early detection.
Prevalence and risk factors
Age-related hypertension affects a significant portion of the older population. According to recent studies, the prevalence of hypertension in adults over the age of 60 ranges from 60% to 90%. Several risk factors contribute to the development of age-related hypertension, including genetics, family history of hypertension, sedentary lifestyle, poor diet, obesity, and certain chronic conditions such as diabetes and kidney disease.
Complications and impact on health
Age-related hypertension can have severe consequences if left uncontrolled. It significantly increases the risks of heart disease, heart attack, stroke, kidney problems, and even cognitive decline. Managing blood pressure and adopting a healthy lifestyle are essential for minimizing these risks and maintaining overall health.
Hypertension in Young Adults
Early-onset hypertension
While hypertension is commonly associated with older adults, it can also affect young adults. Early-onset hypertension refers to high blood pressure that develops at a younger age. It is vital to address and manage hypertension in young adults promptly, as it can lead to long-term health complications if left untreated.
Causes and contributing factors
Various factors contribute to hypertension in young adults. These include genetics, obesity, sedentary lifestyle, poor dietary choices (such as excessive sodium intake), excessive alcohol consumption, smoking, and chronic stress. Identifying and addressing these contributing factors is crucial for effectively managing blood pressure in young adults.
Medical conditions and lifestyle choices
Certain medical conditions, such as kidney disease, hormonal disorders, and chronic conditions like diabetes, can contribute to hypertension in young adults. Additionally, unhealthy lifestyle choices, such as lack of physical activity, an unhealthy diet, and substance abuse, can increase the risk of developing high blood pressure at a young age. Adopting healthy habits and seeking medical intervention when necessary are key to managing hypertension in young adults.
Studies on Age and Blood Pressure
Study 1: Impact of age on blood pressure regulation
A recent study published in the Journal of the American Medical Association investigated the impact of age on blood pressure regulation. The study found that as individuals age, their blood pressure regulation mechanisms become less efficient, leading to higher systolic blood pressure. The researchers emphasized the importance of regular blood pressure monitoring and targeted interventions to prevent age-related hypertension.
Study 2: Age-related changes in arterial structure and blood pressure
Another study conducted at the National Institute on Aging examined age-related changes in arterial structure and their relationship to blood pressure. The study revealed that arterial stiffness and decreased elasticity were significant factors in the development of age-related hypertension. The findings emphasized the importance of maintaining arterial health through lifestyle modifications and medical interventions to prevent high blood pressure.
Study 3: Relationship between age and hypertension risk
A study published in the Journal of Hypertension explored the relationship between age and the risk of developing hypertension. The study demonstrated that age is an independent risk factor for hypertension, highlighting the need for age-specific interventions to prevent and manage high blood pressure. The findings also underscored the importance of early detection and proactive management in minimizing the long-term health implications of age-related hypertension.

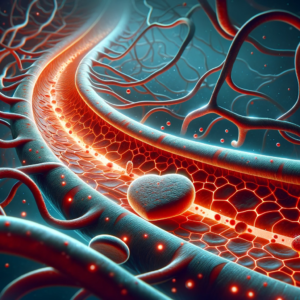
Age-Related Changes in Blood Vessels
Arterial stiffness and elasticity
With age, blood vessels tend to lose their elasticity and become stiffer. This phenomenon, known as arterial stiffness, makes it more difficult for blood to flow smoothly, increasing the workload on the heart and contributing to higher blood pressure levels. Addressing arterial stiffness through lifestyle modifications, regular exercise, and medication can help manage age-related hypertension.
Collagen deposition and vascular remodeling
As people age, there is an increase in collagen deposition in blood vessel walls, which results in vascular remodeling. This remodeling contributes to narrowing and thickening of the blood vessels, further impeding blood flow and elevating blood pressure. Understanding these structural changes is crucial to develop targeted interventions and personalized treatment plans for individuals with age-related hypertension.
Impact of Aging on Blood Pressure Regulation
Renin-angiotensin system
Aging affects the renin-angiotensin system (RAS), a hormonal system involved in blood pressure regulation. With age, the RAS becomes overactive, leading to increased constriction of blood vessels and fluid retention, contributing to elevated blood pressure. Medications that target the RAS, such as angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs), are often prescribed to manage age-related hypertension effectively.
Autonomic nervous system
The autonomic nervous system plays a crucial role in regulating blood pressure. Aging affects the autonomic nervous system, leading to imbalances in sympathetic and parasympathetic activities. These imbalances can result in higher blood pressure levels and reduced cardiovascular adaptability. Managing autonomic dysfunction through lifestyle changes and stress management techniques can help control age-related hypertension.
Endothelial dysfunction
Endothelial dysfunction refers to the impaired functioning of the endothelium, the inner lining of blood vessels. With aging, the endothelium undergoes changes that affect its ability to dilate and constrict blood vessels appropriately. This dysfunction contributes to increased blood pressure and the development of age-related hypertension. Lifestyle modifications, including dietary interventions rich in antioxidants and regular physical activity, can improve endothelial function and help manage blood pressure.
Contributing Factors to Age-Related Hypertension
Genetics
Genetics plays a significant role in a person’s susceptibility to age-related hypertension. Individuals with a family history of high blood pressure are more likely to develop hypertension themselves. Identifying genetic markers and understanding their impact on blood pressure regulation can aid in early detection and personalized treatment strategies.
Lifestyle choices
Unhealthy lifestyle choices can contribute to the development of age-related hypertension. Sedentary behavior, an unhealthy diet high in sodium and saturated fats, excessive alcohol consumption, and tobacco use all increase the risk of elevated blood pressure. Making positive lifestyle changes, such as engaging in regular exercise, adopting a balanced diet, limiting alcohol intake, and quitting smoking, can significantly lower the chances of developing hypertension.
Obesity and weight gain
Obesity and weight gain are significant risk factors for hypertension, especially in older individuals. Excess weight puts additional strain on the cardiovascular system, leading to increased blood pressure. Losing weight through a combination of healthy eating and regular physical activity can help lower blood pressure and reduce the risk of age-related hypertension.
Management and Prevention
Lifestyle modifications
Healthy lifestyle choices play a crucial role in the management and prevention of age-related hypertension. Regular exercise, adopting a balanced diet rich in fruits, vegetables, and whole grains, reducing sodium intake, managing stress effectively, avoiding tobacco use, and limiting alcohol consumption are all recommended lifestyle modifications. These interventions can help lower blood pressure, reduce the risk of complications, and improve overall cardiovascular health.
Antihypertensive medications
In some cases, lifestyle modifications alone may not be sufficient to control blood pressure. Antihypertensive medications may be prescribed by healthcare professionals to manage age-related hypertension effectively. These medications aim to lower blood pressure and reduce the workload on the heart. Commonly prescribed medications include diuretics, ACE inhibitors, ARBs, beta-blockers, and calcium channel blockers. It is essential to work closely with a healthcare provider to determine the most appropriate medication regimen for individual needs.
Regular blood pressure monitoring
Regular blood pressure monitoring is crucial for managing and preventing age-related hypertension. Checking blood pressure at home using a reliable blood pressure monitor and regular visits to healthcare professionals for comprehensive check-ups are vital. Monitoring blood pressure allows for early detection of changes, facilitates prompt intervention, and provides valuable information for assessing the effectiveness of treatment strategies.
In conclusion, understanding how age affects blood pressure is essential for maintaining cardiovascular health and preventing related complications. Age-related changes in the cardiovascular system, along with genetic and lifestyle factors, contribute to the development of hypertension. Regular blood pressure monitoring, adopting a healthy lifestyle, and appropriate medical interventions are key to managing and preventing age-related hypertension effectively. By taking proactive steps to control blood pressure as we age, we can promote long-term cardiovascular well-being and enjoy a healthier, more fulfilling life.