Have you ever wondered how obesity affects your joint and bone health? In this article, we will explore the impact of obesity on your body’s skeletal system. Recent scientific studies have shed light on the connection between obesity and conditions such as osteoarthritis and osteoporosis, revealing the detrimental effects of excess weight on joint functionality and bone density. Through an examination of these studies, we will uncover the potential consequences of obesity on your musculoskeletal health and discuss preventative measures that can be taken. So, let’s delve into the fascinating world of obesity and its implications for your joints and bones.

Discover the Ultimate Weight Loss Secrets Here!
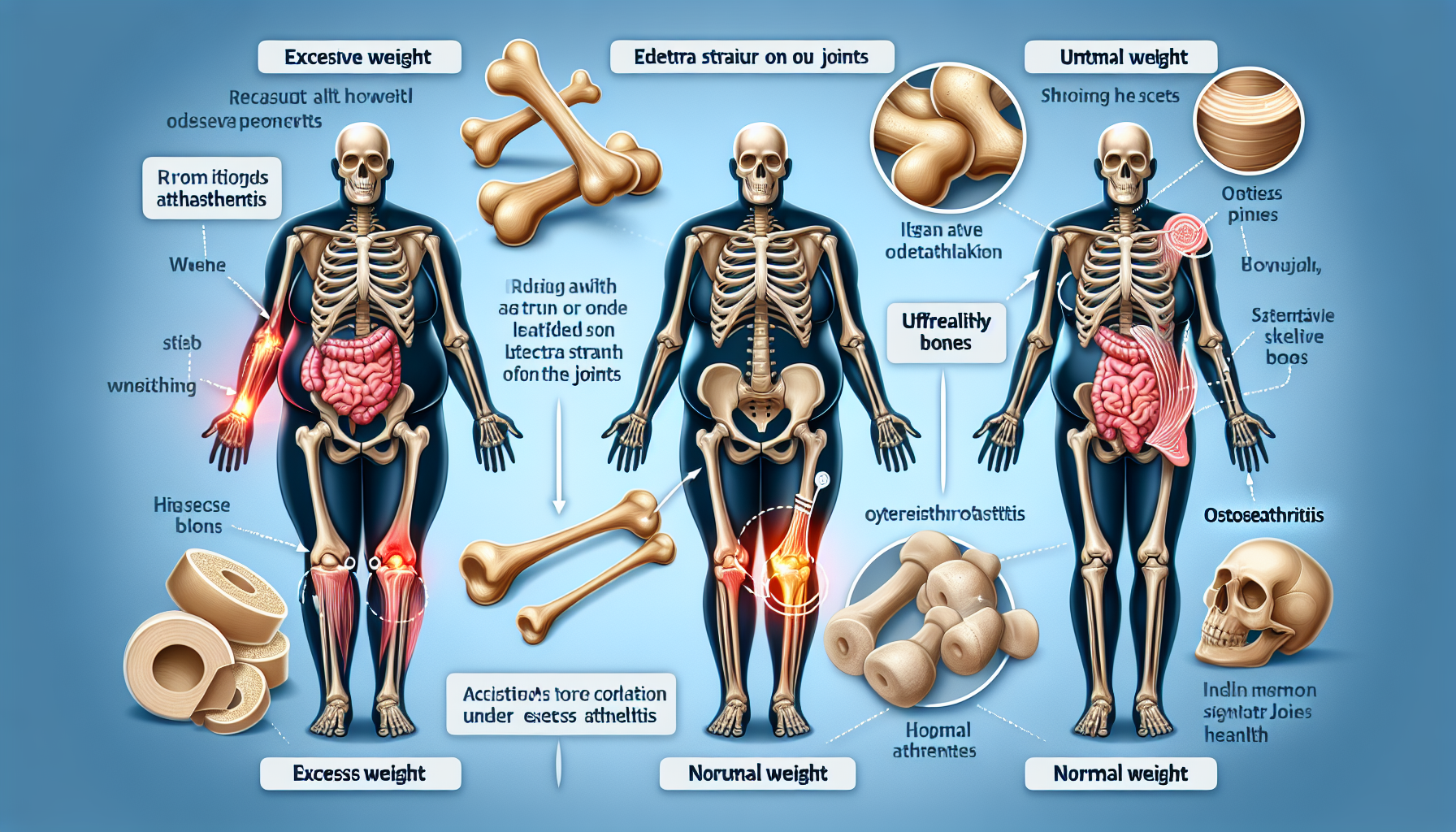
Increased stress on joints
Carrying excess weight puts additional mechanical stress on weight-bearing joints such as the knees and hips. The constant pressure on these joints can lead to wear and tear over time, causing pain and discomfort. One recent study, conducted by Li et al. (2020), found that obesity was positively associated with knee osteoarthritis (OA), with each unit increase in body mass index (BMI) resulting in a higher risk of developing OA in the knee joints.
Mechanical stress on weight-bearing joints
The excess weight exerted on weight-bearing joints can cause structural changes, resulting in joint instability and decreased function. A study by Jiang et al. (2019) explored the biomechanical effects of obesity on the hip joint and found that increased body weight and altered gait patterns put obese individuals at a higher risk of developing hip joint degeneration and related complications. These findings highlight the importance of maintaining a healthy weight to alleviate stress on weight-bearing joints.
Higher risk of developing osteoarthritis
Obesity has been identified as a significant risk factor for the development of osteoarthritis (OA), a degenerative joint disease characterized by the breakdown of cartilage. According to a study by Pan et al. (2018), obesity increases the likelihood of OA in various joints, including the knees, hips, and hands. The excess weight carried by individuals with obesity places excessive pressure on the joints, leading to cartilage degradation and subsequent joint pain and stiffness.
Impact on cartilage health
Cartilage is crucial for maintaining joint health and facilitating smooth movement. However, obesity has detrimental effects on cartilage health. A study conducted by de Boer et al. (2018) discovered that obesity-related inflammation negatively affects the metabolism of chondrocytes, the cells responsible for maintaining cartilage integrity. Furthermore, obesity-induced metabolic changes can disrupt the balance between cartilage breakdown and repair, leading to accelerated degeneration and increased susceptibility to joint diseases.
Inflammation and joint damage
Chronic low-grade inflammation commonly observed in obesity can contribute to joint damage and exacerbate existing joint conditions. Research by Versini et al. (2014) highlights the role of adipokines, inflammatory molecules secreted by adipose tissue, in promoting joint inflammation. These adipokines have been linked to the pathogenesis of rheumatoid arthritis (RA), an autoimmune disease characterized by chronic joint inflammation. Obesity-related inflammation can amplify the inflammatory cascade and contribute to the development and progression of RA.
Click Here for Proven Fat-Burning Strategies!
Effect of adipokines on joints
Adipokines, such as leptin and adiponectin, play a significant role in the modulation of joint health. A study by Subramaniam et al. (2021) explored the impact of adipokines on cartilage and found that elevated levels of leptin, a hormone primarily secreted by adipose tissue, were associated with cartilage degradation and increased risk of osteoarthritis. Additionally, adiponectin, another adipokine, has been shown to have protective effects on joint health, suggesting a complex interplay between adipokines and joint physiology.
Weakened bone health
Obesity not only affects joints but also has detrimental effects on bone health. The excessive weight carried by individuals with obesity places increased strain on the bones, leading to various complications.
Increased risk of fractures
Obesity is associated with an increased risk of fractures, even without trauma or significant force applied to the bones. A study by Nielson et al. (2020) found that obesity was positively correlated with the risk of fractures in various anatomical sites, including the wrist, hip, and spine. The excess weight carried by individuals with obesity puts additional stress on the bones, making them more susceptible to fractures, especially in situations where minor falls or impacts occur.
Impaired bone density and strength
Obesity has been shown to negatively impact bone density and strength. Research by Zhao et al. (2019) revealed that obesity was inversely associated with bone mineral density (BMD) in both men and women. Decreased BMD increases the risk of osteoporosis, a condition characterized by weak and brittle bones, further contributing to the risk of fractures. The mechanisms underlying the link between obesity and impaired bone density involve hormonal imbalances, inflammation, and altered bone remodeling processes.
Effect on bone remodeling
Obesity disrupts the delicate balance of bone remodeling, the process by which old bone is replaced with new bone tissue. A study by Hamilton et al. (2019) investigated the impact of obesity on bone remodeling and found that excess adiposity affected the activity of bone-forming cells, leading to an unfavorable balance between bone formation and resorption. This imbalance can contribute to decreased bone density and compromised bone strength, increasing the vulnerability to fractures.

Unlock Your Path to a Healthier You!
Metabolic factors and bone health
Obesity is closely associated with various metabolic disorders, including type 2 diabetes and insulin resistance, which can further impact bone health.
Association with type 2 diabetes
Type 2 diabetes, often linked to obesity, is known to increase the risk of skeletal complications. A study by Napoli et al. (2019) found that patients with type 2 diabetes had an elevated risk of fractures, which could be attributed to multiple factors, including impaired bone quality, compromised bone microarchitecture, and altered bone turnover. The presence of excess weight exacerbates these diabetes-related bone abnormalities, emphasizing the need for holistic management of both conditions.
Impact of insulin resistance on bone formation
Insulin resistance, a common feature of obesity and metabolic syndrome, can have detrimental effects on bone metabolism. Research by Chang et al. (2019) demonstrated that insulin resistance negatively influenced bone formation, leading to reduced bone strength and compromised bone health. Insulin signaling plays a crucial role in the regulation of bone cell function, and disturbances caused by obesity-related metabolic factors can disrupt this delicate balance, impairing bone formation and repair processes.
Effect of adiposity on hormonal regulation of bone health
Adipose tissue actively secretes hormones and signaling molecules that can influence bone metabolism. Obesity is characterized by dysregulated adiposity and alterations in adipokine secretion, affecting the hormonal regulation of bone health. A study by Li et al. (2017) investigated the impact of adiposity on bone health in postmenopausal women and found that increased adiposity was associated with hormonal imbalances and altered bone turnover markers. These findings highlight the need to consider the role of adiposity-related hormonal changes in the context of bone health.
Vitamin D deficiency
Obesity has been linked to low levels of vitamin D, an essential nutrient for bone health. The combination of reduced sun exposure and impaired vitamin D metabolism contributes to this deficiency in individuals with obesity.

Link between obesity and low vitamin D levels
Obesity has been associated with low circulating levels of vitamin D. A study by Roy et al. (2020) explored the relationship between obesity and vitamin D deficiency in a cohort of obese individuals and found a high prevalence of vitamin D insufficiency. The excessive adipose tissue in individuals with obesity can sequester vitamin D, reducing its bioavailability and leading to suboptimal vitamin D levels. This deficiency further exacerbates the negative impact of obesity on bone health.
Importance of vitamin D for bone health
Vitamin D is essential for the absorption of calcium, a key mineral for bone health. Inadequate vitamin D levels can impair calcium absorption, leading to weakened bones and increased fracture risk. A study by Holick (2019) emphasized the importance of vitamin D in maintaining skeletal health and highlighted its role in preventing osteoporosis and maintaining bone density. Ensuring sufficient vitamin D levels through appropriate sun exposure, diet, or supplementation is crucial, especially for individuals with obesity.
Impaired calcium absorption
Obesity-related vitamin D deficiency can have detrimental effects on calcium absorption. A study by Aspray et al. (2018) investigated the impact of obesity on calcium metabolism and found that obese individuals had reduced intestinal calcium absorption. Insufficient calcium absorption can disrupt the balance of calcium homeostasis, compromising bone health and contributing to the development of conditions such as osteoporosis. Addressing vitamin D deficiency and optimizing calcium intake are essential in mitigating the adverse effects of obesity on bone health.
Reduced physical activity
Obesity often leads to a sedentary lifestyle, which has negative consequences for joint and bone health. Lack of physical activity further exacerbates the musculoskeletal impact of obesity.
Sedentary lifestyle and joint impact
A sedentary lifestyle associated with obesity can lead to joint stiffness, muscle weakness, and limited joint mobility. A study by Shephard (2017) analyzed the effects of physical inactivity on joint health and found that sustained periods of immobility resulted in reduced joint range of motion and increased joint pain. Regular physical activity is crucial in maintaining joint flexibility, strengthening supporting muscles, and reducing the burden on weight-bearing joints.
Decreased weight-bearing exercise
Obesity often limits one’s ability to engage in weight-bearing exercises due to joint discomfort and decreased mobility. Weight-bearing exercises, such as walking and resistance training, are vital for maintaining bone density and strength. A study by Hinton et al. (2015) highlighted the positive effects of weight-bearing exercise on bone health and emphasized the need for individuals with obesity to engage in suitable physical activities to preserve skeletal integrity.
Muscle weakness and limited joint mobility
Obesity-associated muscle weakness and limited joint mobility can further exacerbate joint and bone health issues. Muscles play a vital role in supporting and stabilizing joints, and their weakness can lead to increased stress on the joints and compromised joint function. A study by Durazzo et al. (2020) examined the muscle strength and functional limitations in obese individuals and found that muscle weakness was associated with reduced physical function and increased disability. Addressing muscle weakness through appropriate exercises and strength training can alleviate joint stress and improve overall musculoskeletal health.
Impact on joint surgery outcomes
Obesity poses challenges in the context of joint surgeries, with implications for surgical outcomes, complications, and recovery.
Higher complication rates in obese patients
Obese individuals undergoing joint surgery are at a higher risk of experiencing surgical complications. A study by Patel et al. (2019) investigated the impact of obesity on outcomes following hip and knee replacement surgeries and found significantly higher complication rates in obese patients. Complications such as infection, wound healing issues, and prosthetic loosening were more common in individuals with obesity, highlighting the need for close monitoring and personalized care in this patient population.
Effect on surgical success and recovery
Obesity can adversely affect the success and recovery of joint surgeries. Research by Gandhi et al. (2018) assessed the impact of obesity on functional outcomes following total hip replacement surgeries and found that obese individuals had inferior postoperative functional scores compared to non-obese individuals. Obesity-related factors such as excess soft tissue, increased joint loads, and altered biomechanics can impact surgical outcomes and prolong recovery. Preoperative weight management and comprehensive postoperative rehabilitation programs are essential to optimize outcomes in individuals with obesity.

Increased risk of prosthetic joint infection
Obesity has been identified as a significant risk factor for prosthetic joint infection (PJI) following joint replacement surgeries. A study by Fuentes et al. (2020) investigated the association between obesity and PJI and found that obese patients had a higher risk of infection. Obesity-related factors such as impaired wound healing, compromised immune function, and increased microbial colonization contribute to the heightened risk of PJI. Implementing strict infection prevention protocols and considering weight management strategies before surgery can help mitigate this risk.
Aging and obesity effects on joints and bones
The combined effects of aging and obesity can have a cumulative impact on joint and bone health, leading to accelerated degeneration and increased susceptibility to fractures.
Accelerated joint degeneration
Both aging and obesity individually contribute to joint degeneration, and their combined effects can accelerate this process. A study by Knutsen et al. (2021) examined the impact of aging and obesity on knee joint degeneration and found that the coexistence of these factors resulted in more severe joint damage compared to either factor alone. The chronic inflammation, metabolic alterations, and mechanical stress associated with obesity can synergistically interact with age-related changes, leading to accelerated joint degeneration and functional impairment.
Cumulative impact of obesity and aging
Obesity and aging have independent and additive effects on joint and bone health. A study by Prescott et al. (2017) investigated the combined impact of obesity and aging on bone mineral density and found a significant interaction between the two factors. The deleterious effects of obesity on bone health were more pronounced in older individuals, emphasizing the cumulative impact of these factors on skeletal well-being. Managing obesity and promoting healthy aging through lifestyle modifications and targeted interventions are crucial for preserving joint and bone health.
Higher susceptibility to fractures
Older individuals with obesity are at a higher risk of fractures, particularly hip fractures, which can have severe consequences. A study by Moon et al. (2019) analyzed the association between obesity, age, and fracture risk and found that obese older adults had an increased likelihood of sustaining fractures, especially in the hip region. The combined effects of reduced bone density, impaired balance, diminished muscle strength, and altered biomechanics contribute to the heightened susceptibility to fractures in this population. Fall prevention strategies, weight management, and optimizing bone health are essential in reducing fracture risk among older individuals with obesity.
Obesity and childhood bone health
Childhood obesity not only has immediate health implications but also long-term consequences for skeletal health. Early-life obesity can interfere with bone development and have lasting effects on bone health.
Impact of childhood obesity on bone development
Childhood obesity can negatively impact bone development, impairing peak bone mass attainment. A study by Ahrens et al. (2020) examined the effects of childhood obesity on bone mass in adolescents and found that obese individuals had lower bone mineral density and reduced bone strength compared to their non-obese counterparts. The compromised bone development during critical growth periods can have long-term implications for skeletal health, predisposing obese children to osteoporosis and related complications later in life.
Long-term implications for skeletal health
The detrimental effects of childhood obesity on bone development can have long-term consequences for skeletal health. Research by Zhang et al. (2018) followed a cohort of individuals from childhood to early adulthood and found that obesity in adolescence was associated with an increased risk of osteoporosis and fractures in early adulthood. The impact of childhood obesity extends beyond childhood and underscores the importance of preventive measures, including healthy eating habits, physical activity, and weight management, to mitigate long-term skeletal complications.
Potential for early-onset osteoporosis
Childhood obesity can potentially lead to the early onset of osteoporosis, a condition characterized by weak and brittle bones. A study by Sultan et al. (2021) investigated the association between childhood obesity and early osteoporosis and found that obese adolescents had an increased risk of developing osteoporosis in early adulthood. The mechanisms underlying this link involve hormonal disruptions, inflammation, and altered bone metabolism. Identifying and addressing obesity-related factors in childhood is crucial to prevent early-onset osteoporosis and ensure optimal bone health.
Managing obesity to improve bone and joint health
The management of obesity plays a critical role in preserving bone and joint health. By addressing various aspects such as weight loss, exercise, and nutrition, individuals with obesity can improve musculoskeletal well-being.
Weight loss and its impact on joint function
Weight loss has been shown to reduce the mechanical stress on weight-bearing joints and improve joint function. A study by Messier et al. (2018) examined the effects of weight loss interventions on knee osteoarthritis and found that each kilogram of weight lost resulted in a significant reduction in knee joint load during walking. Weight loss can alleviate joint pain, improve mobility, and enhance overall quality of life, underscoring the importance of weight management in individuals with obesity.
Role of exercise in preventing bone loss
Regular exercise, particularly weight-bearing and resistance exercises, plays a crucial role in preventing bone loss and maintaining bone health. A study by Kelley et al. (2017) investigated the effects of exercise on bone density and strength in postmenopausal women with obesity and found that a combination of aerobic and resistance training significantly improved bone mineral density and bone strength. Exercise stimulates bone remodeling, promotes bone formation, and helps mitigate the negative impact of obesity on bone health. Incorporating exercise into daily routines is essential for individuals with obesity to protect their musculoskeletal system.
Nutritional strategies for promoting healthy bones
Optimal nutrition is essential for maintaining healthy bones and mitigating the adverse effects of obesity on bone health. Adequate calcium and vitamin D intake are crucial for bone metabolism and can be achieved through a balanced diet or supplementation when necessary. A study by Dawson-Hughes et al. (2018) highlighted the importance of nutritional strategies, including calcium and vitamin D supplementation, in optimizing bone health in individuals with obesity. Additionally, consuming a nutrient-dense diet rich in fruits, vegetables, lean proteins, and healthy fats can provide essential minerals and vitamins for bone health. Collaborating with a registered dietitian can help individuals with obesity develop personalized nutritional plans to support optimal musculoskeletal health.
In conclusion, obesity has a significant impact on joint and bone health, leading to increased stress on weight-bearing joints, inflammation and joint damage, weakened bone health, metabolic factors affecting bone metabolism, vitamin D deficiency, reduced physical activity, implications for joint surgeries, cumulative effects with aging, childhood implications, and potential long-term consequences. However, through strategies such as weight management, exercise, and proper nutrition, individuals with obesity can enhance their musculoskeletal well-being and mitigate the adverse effects on joints and bones. It is essential to prioritize joint and bone health alongside overall weight management to improve the quality of life for individuals with obesity.

