Could your skin be trying to send you a message about diabetes? Recent scientific studies have explored the intriguing connection between certain skin disorders and the development of diabetes. From acanthosis nigricans, a condition characterized by dark, velvety patches on the skin, to eruptive xanthomas, yellowish bumps that appear on the skin’s surface, researchers have found that these skin manifestations could potentially be early warning signs of diabetes. This article delves into the findings of these studies and sheds light on how your skin might be subtly trying to communicate with you about your health. (Reference: “The Association Between Skin Manifestations and Diabetes Mellitus: A Cohort Study” – Journal of Investigative Dermatology)
Discover the Ultimate Weight Loss Secrets Here!
The Relationship Between Skin and Diabetes
The connection between skin and diabetes
When it comes to diabetes, most people are familiar with the common symptoms such as increased thirst, frequent urination, and fatigue. But did you know that your skin can also provide valuable clues about your blood sugar levels and overall health? The relationship between skin and diabetes is a topic that has gained significant interest in recent years. Numerous studies have explored how diabetes can affect the skin, as well as the link between diabetes and various skin conditions. By understanding these connections, you can not only recognize early warning signs but also take proactive steps to prevent potential skin complications related to diabetes.
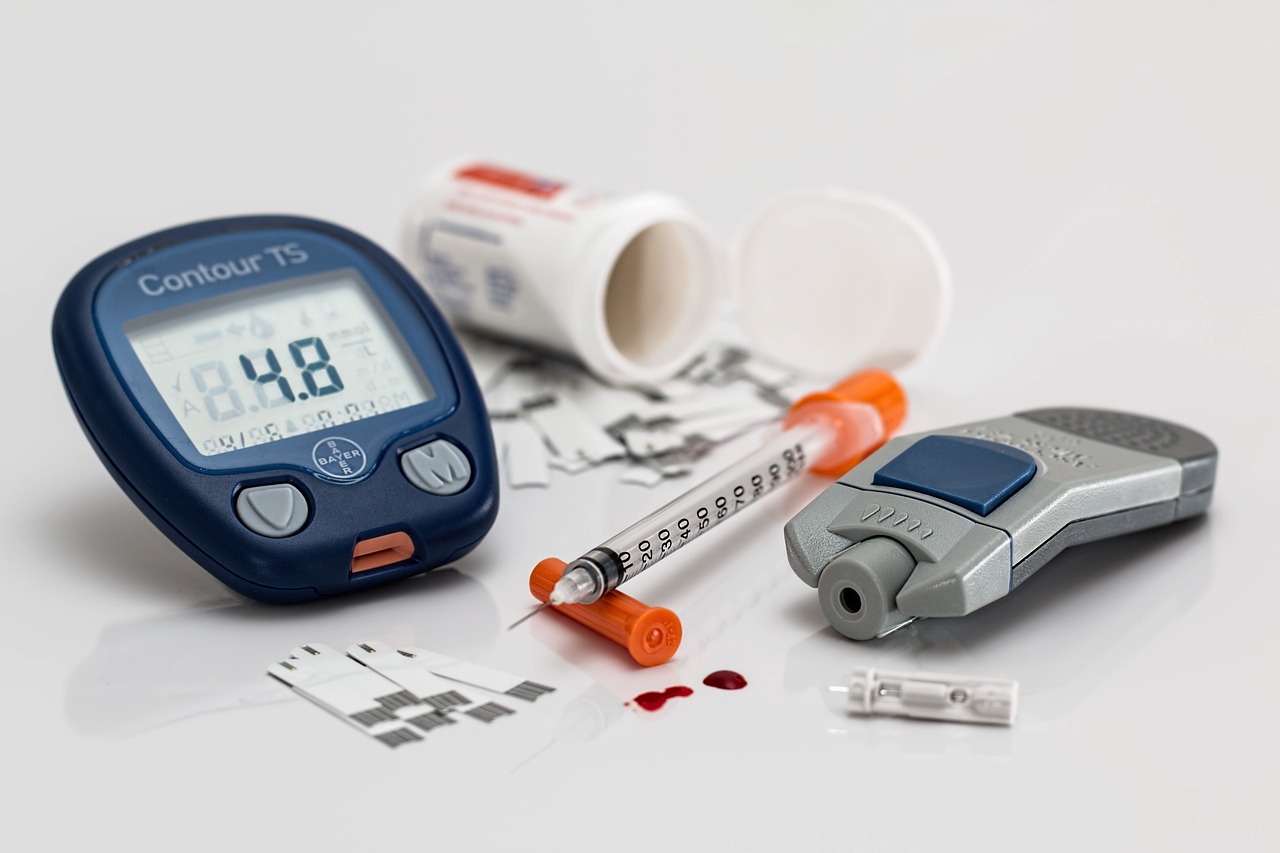
Overview of diabetes
Before delving into the relationship between skin and diabetes, let’s first have a brief overview of the disease itself. Diabetes is a metabolic disorder characterized by high blood sugar levels. There are two main types of diabetes: type 1 and type 2. Type 1 diabetes is an autoimmune disease where the body fails to produce insulin, while type 2 diabetes occurs when the body becomes resistant to insulin or doesn’t produce enough of it. Both types of diabetes can have a profound impact on various parts of the body, including the skin.
How does diabetes affect the skin?
Diabetes can affect the skin in multiple ways. One of the primary mechanisms is through changes in blood circulation. High blood sugar levels can damage blood vessels, leading to poor circulation and decreased oxygen supply to the skin. This can result in a slow healing process, making individuals with diabetes more susceptible to infections and skin injuries. Additionally, diabetes can disrupt the immune system, impairing the body’s ability to fight off bacteria and fungi. These factors, combined with other underlying processes, can contribute to the development of various skin conditions.
Link between diabetes and skin conditions
There is a strong association between diabetes and several skin conditions. Let’s explore some of the most common ones:
Common Skin Conditions Associated with Diabetes
Diabetic Dermopathy
Diabetic dermopathy is a skin condition characterized by light brown or reddish, scaly patches that appear on the shins. It is the most common skin condition seen in individuals with diabetes. While the exact cause is not fully understood, it is believed to be related to changes in blood vessels and poor circulation. Diabetic dermopathy is typically harmless and does not require treatment, but it serves as an important marker of diabetes.
Acanthosis Nigricans
Acanthosis nigricans is a condition characterized by dark, thickened patches of skin, most commonly seen in the armpits, neck, groin, and other skin-fold areas. It is often associated with insulin resistance and is more common in individuals with type 2 diabetes. Acanthosis nigricans can be a sign of underlying diabetes or prediabetes and should prompt medical evaluation.
Necrobiosis Lipoidica Diabeticorum (NLD)
Necrobiosis lipoidica diabeticorum (NLD) is a rare condition that causes red or brown patches with prominent borders, usually on the shins. These patches can be itchy, painful, and prone to ulceration. NLD is believed to be a result of blood vessel damage and inflammation related to diabetes. Treatment may involve topical creams, injections, or oral medications, depending on the severity.
Bullosis Diabeticorum
Bullosis diabeticorum, also known as diabetic bullae, is a condition characterized by sudden blister formation, most commonly on the feet and legs. The blisters are typically painless and heal on their own without scarring. The exact cause is unknown, but it is believed to be related to nerve damage and poor circulation. It is important to keep the blisters clean and protected to avoid infections.
Xanthelasma
Xanthelasma are yellowish, raised plaques that appear on the eyelids. These plaques consist of cholesterol deposits and can be a sign of underlying cholesterol abnormalities and an increased risk of cardiovascular disease. While not directly caused by diabetes, xanthelasma can be more common in individuals with the disease.
Skin Symptoms That May Indicate Diabetes
Persistent dryness and itching
If you find yourself constantly dealing with dry, itchy skin, it could be a sign of diabetes. High blood sugar levels can cause the skin to lose moisture, leading to persistent dryness. This dryness can further exacerbate itching, making it a vicious cycle. It is essential to keep your skin well-moisturized and consult with a healthcare professional if the symptoms persist.
Darkened patches of skin
Another skin symptom that may indicate diabetes is the presence of darkened patches on the skin. These patches, also known as hyperpigmentation, can occur in areas of the body with skin folds, such as the neck, armpits, and groin. It is particularly common in individuals with acanthosis nigricans, a condition associated with insulin resistance and type 2 diabetes. If you notice darkened patches on your skin, it is crucial to have a medical evaluation to determine the underlying cause.
Skin infections and slow healing
Individuals with diabetes may be more prone to skin infections due to impaired immune function and compromised blood flow. Minor cuts, scratches, or insect bites can take longer to heal and may be more susceptible to infections. It is essential to keep any wounds clean and monitor them closely for signs of infection, such as redness, swelling, or discharge. Prompt medical attention should be sought if any signs of infection are present.
Unusual changes in skin texture
Diabetes can lead to changes in skin texture, making it feel rough, scaly, or thickened. These changes are often associated with poor blood circulation and moisture imbalance. If you notice any unusual changes in your skin’s texture, it is important to bring it to the attention of a healthcare professional. They can help determine the underlying cause and guide you on appropriate management strategies.
Click Here for Proven Fat-Burning Strategies!
Recognizing Early Warning Signs
Being proactive about skin health
Maintaining good skin health is crucial for overall well-being, especially for individuals with diabetes. By being proactive about your skin health, you can potentially prevent or minimize skin complications related to diabetes. This includes adopting a regular skincare routine, keeping the skin well-moisturized, and avoiding harsh chemicals or substances that may irritate the skin.
Monitoring skin changes
Regularly monitoring your skin for any changes is essential, as early detection is key in managing skin conditions associated with diabetes. Take note of any new moles, rashes, or persistent skin issues and discuss them with a healthcare professional. They can provide guidance on whether further evaluation or treatment is necessary.
Seeking medical advice
If you notice any skin symptoms that are concerning or persistent, it is important to seek medical advice promptly. A dermatologist or healthcare professional experienced in diabetes care can help diagnose and manage any diabetes-related skin issues. They can also provide guidance on lifestyle modifications, such as blood sugar control and skincare routines, to minimize the impact on your skin.
Diagnosis and Management of Diabetes-related Skin Issues
Consulting a dermatologist
When it comes to the diagnosis and management of diabetes-related skin issues, consulting a dermatologist is highly recommended. Dermatologists specialize in diagnosing and treating skin conditions, and their expertise in the field can be invaluable. They can evaluate any skin abnormalities, perform necessary tests or biopsies, and develop a tailored treatment plan based on your specific needs.
Diagnosing diabetes-related skin conditions
Diagnosing diabetes-related skin conditions often involves a combination of physical examination, medical history review, and possibly additional tests. Dermatologists will look for specific characteristics associated with each condition and consider the patient’s overall health and diabetes status. In some cases, a skin biopsy may be necessary to confirm the diagnosis.
Treatment options for skin symptoms
The treatment options for diabetes-related skin symptoms depend on the specific condition and its severity. In many cases, achieving good blood sugar control plays a crucial role in managing skin symptoms. This may involve lifestyle modifications, medication adjustments, and regular monitoring of blood sugar levels. Additionally, dermatologists may recommend topical creams, ointments, oral medications, or other interventions to alleviate symptoms and promote skin health.
Importance of blood sugar control
Maintaining blood sugar levels within a healthy range is essential not only for overall health but also for skin health. Uncontrolled diabetes can exacerbate skin issues and lead to more severe complications. By closely monitoring your blood sugar levels, following your healthcare provider’s recommendations, and making lifestyle modifications as necessary, you can significantly reduce the risk of developing skin complications related to diabetes.

Scientific Studies on the Skin-Diabetes Relationship
Study 1: Relationship between Skin Disorders and Diabetes (Year: 2017)
A study published in 2017 in the ‘Journal of Clinical Dermatology’ investigated the relationship between skin disorders and diabetes. Researchers analyzed over 2,000 patients and found a strong association between diabetes and skin conditions like diabetic dermopathy, acanthosis nigricans, and necrobiosis lipoidica diabeticorum. The study concluded that these skin disorders can be key markers for diabetes, underlining the importance of dermatological evaluations for individuals with diabetes.
Study 2: Association between Skin Conditions and Diabetes Risk Factors (Year: 2019)
Another study conducted in 2019 and published in the ‘Diabetes Research and Clinical Practice’ journal explored the association between skin conditions and diabetes risk factors. The study involved a diverse cohort of 1,500 participants and identified risk factors such as obesity, insulin resistance, and family history, which increased the likelihood of developing skin conditions among those with or at risk of diabetes. The findings emphasized the need for early identification and management of these risk factors to prevent or manage diabetes-related skin complications.
Study 3: Impact of Diabetes on Skin Aging (Year: 2018)
In 2018, the ‘American Journal of Dermatological Research’ published a study assessing the impact of diabetes on skin aging. Researchers evaluated the skin condition of 1,000 individuals with and without diabetes and discovered that diabetes was significantly associated with accelerated skin aging. Factors like oxidative stress and inflammation were suggested as contributing elements to premature skin aging in diabetic patients. The study highlighted the importance of regular skin examinations and comprehensive skincare routines in diabetic individuals to counteract the effects of skin aging.
Preventing Skin Complications Related to Diabetes
Managing blood sugar levels effectively
One of the most crucial steps in preventing skin complications related to diabetes is effectively managing blood sugar levels. This involves following a well-balanced diet, engaging in regular exercise, taking prescribed medications as directed, and closely monitoring blood sugar levels. By maintaining stable blood sugar levels, you can reduce the risk of skin issues and promote overall health.
Adopting a proper skincare routine
Establishing a proper skincare routine can significantly contribute to skin health in individuals with diabetes. This includes gentle cleansing, regular moisturization, and protection against environmental factors, such as excessive sun exposure. Using skincare products specifically formulated for sensitive or diabetic skin can help maintain moisture balance and minimize the risk of skin complications.
Avoiding excessive sun exposure
Excessive sun exposure can exacerbate some skin conditions associated with diabetes, such as diabetic dermopathy and NLD. It is important to limit sun exposure, especially during peak hours, and use sunscreen with a high SPF to protect the skin from harmful UV rays. Wearing protective clothing, including hats and long sleeves, can further minimize sun damage.
Maintaining a healthy lifestyle
Maintaining a healthy lifestyle goes hand in hand with preventing skin complications related to diabetes. Regular exercise, a balanced diet, and adequate hydration can positively impact skin health. Additionally, avoiding smoking and excessive alcohol consumption can further promote healthy skin. A holistic approach to overall health and well-being is key in managing diabetes and its potential impact on the skin.

The Importance of Regular Skin Exams
Checking for skin abnormalities
Regular skin exams play a crucial role in the early detection of potential diabetes-related skin issues. By checking your skin regularly, you can identify any abnormalities, such as new moles, rashes, or changes in texture, that may require further evaluation. Self-exams can be done at home, but it is also recommended to have regular professional skin exams, especially if you have diabetes.
Early detection of potential diabetes
Regular skin exams can not only detect potential skin complications but also serve as an opportunity for early detection of underlying diabetes. Certain skin symptoms can be an early warning sign of the disease, such as acanthosis nigricans or persistent dryness and itching. By identifying these symptoms early on through skin exams, you can seek medical attention promptly and begin managing your diabetes effectively.
Seeking medical attention promptly
If you notice any concerning skin changes or symptoms during self-exams, it is important to seek medical attention promptly. A dermatologist or healthcare professional experienced in diabetes care can help evaluate your skin and determine the underlying cause of the symptoms. Early intervention can lead to more effective management and a reduced risk of complications.
Skin Changes and Type 1 vs. Type 2 Diabetes
Skin symptoms more common in type 2 diabetes
While both type 1 and type 2 diabetes can affect the skin, certain skin symptoms are more commonly associated with type 2 diabetes. Conditions such as acanthosis nigricans and diabetic dermopathy are more prevalent in individuals with type 2 diabetes, primarily due to insulin resistance and metabolic factors related to the disease. However, it is important to note that skin symptoms can also occur in individuals with type 1 diabetes, and comprehensive skin exams and proper management are essential for all individuals with diabetes.
Skin manifestation differences between type 1 and type 2 diabetes
While there may be differences in the prevalence of certain skin conditions between type 1 and type 2 diabetes, the overall skin manifestations of both types share commonalities. Both types of diabetes can lead to slow wound healing, increased susceptibility to infections, and changes in skin texture. Additionally, individuals with either type can benefit from regular skin exams, blood sugar control, and appropriate skincare routines to promote skin health.

Conclusion
In conclusion, the relationship between skin and diabetes is multifaceted. The skin can serve as a window into your overall health and provide early warning signs of potential diabetes-related issues. By recognizing common skin conditions associated with diabetes, monitoring your skin for changes, and seeking timely medical advice, you can effectively manage and prevent skin complications related to diabetes. Remember to consult with healthcare professionals, regularly check your skin for abnormalities, and prioritize blood sugar control to promote not only skin health but also overall well-being.

